SourcesAll content published on Kenhub is reviewed by medical and anatomy experts. The information we provide is grounded on academic literature and peer-reviewed research.
References:
Illustrators:
Scalene muscles: want to learn more about it?
Our engaging videos, interactive quizzes, in-depth articles and HD atlas are here to get you top results faster.
What do you prefer to learn with?
“I would honestly say that Kenhub cut my study time in half.” – Read more.  Kim Bengochea, Regis University, Denver © Unless stated otherwise, all content, including illustrations are exclusive property of Kenhub GmbH, and are protected by German and international copyright laws. All rights reserved.
Kim Bengochea, Regis University, Denver © Unless stated otherwise, all content, including illustrations are exclusive property of Kenhub GmbH, and are protected by German and international copyright laws. All rights reserved.
Register now and grab your free ultimate anatomy study guide! Info
Grounded on academic literature and research, validated by experts, and trusted by more than 2 million users. Read more.
Copyright © 2022 Kenhub. All rights reserved.
An increase in tone or thickness of the anterior scalene muscle may result in distant symptoms. Vascular compression of the subclavian artery would give pallor and cold sensation to the extremities, cyanosis, and difficulty using the arm. If C5-C6 crosses the muscle in non-physiological conditions (hypertrophy, shortening), it could cause paresthesia, anesthesia, or weakness of the muscles innervated by these roots. If the root of C8 runs back to the two attacks, the anterior scalene, and there is a squeeze, there may be symptoms such as tingling, pain, and weakness of the hand and the interosseous muscles. If the anterior scalene tendon mixes with the longus capitis muscle, headaches may occur.
In patients with COPD, the diaphragm muscle is weakened, flattened, and during the inhalation position, it forces the accessory respiratory muscles to intervene with greater emphasis. What happens to the scalene muscles? An inverse relationship between the thickness of the diaphragm muscle and the thickness of the scalene muscles has been demonstrated: the decreased thickness of the diaphragm and increased hypertrophy of the scalene muscles. Generally, the latter is rich in red or aerobic fibers, but if subjected to constant work, bearing a greater load, the red fibers increase their mass, both as proteins and as quantities of mitochondria and enzymes, capillaries. COPD is an aggravating disease, and the scalene muscles increase the tone and volume not only for hypertrophy but the chronic shortening of the muscles themselves. The first ribs are in an inspiratory attitude, with the pulmonary dome in constant tension. During inspiration, the dome will have difficulty moving downward, further complicating the respiratory act by decreasing the pulmonary vital capacity.
In subjects exhibiting a posture with a forward head position, they demonstrate a greater pain sensitivity, particularly for the trapezius and the scalenus medius; these muscles also demonstrate less range of motion in such cases.[11] Probably, a manual approach to improve the functional capacity of the scalenus medius (and trapezius) could improve the daily posture of the head and neck. The presence of a forward head posture could be related to cervicogenic headache pain.[12]
Electromyography can be used in suspected thoracic outlet syndrome and other clinical settings. In patients with temporomandibular joint dysfunction, it has been shown that anterior scalene has greater electrical activity than people without mandibular joint problems. This could be useful information for the physiotherapist or the osteopath. We know that a dysfunction of the scalene muscles reduces the ventilatory capacity of the patients, and a mandibular disorder could be a symptom rather than the cause.
There have been case reports of various forms of TOS occurring secondary to a hypertrophic anterior scalene muscle.[5] In some cases, it is necessary to eliminate the scalene, either the anterior or middle (i.e., a scalenectomy) muscles. In the presence of abnormal muscle bundles that can compress the vascular-nervous brachial package, identified with ultrasound (“wedge-sickle sign”), the patient must undergo muscular resection. In certain situations when the pathology is secondary to the scalene muscle itself, symptoms can be acutely managed with type A botulinum toxin (botox) injections. These are also helpful in older patients that may need to delay surgery.[6] In specific situations of spasmodic torticollis or cervical dystonia, botox injections can help mitigate symptoms as well.
Clinical Relevance of the Scalene Muscles
The brachial plexus courses between the bellies of the anterior scalene and middle scalene muscles. In upper limb surgery, the brachial plexus can be infiltrated with local anaesthetic to avoid the use of a general anaesthetic – known as an interscalene block.
To do this, local anaesthetic is injected between these muscles at the level of the cricoid cartilage.
The scalene muscles collectively act to elevate the first and second ribs, and in doing so they increase the intrathoracic volume. In patients with respiratory distress, the scalene muscles may be used as ‘accessory muscles of respiration’ to aid with breathing.
By increasing intrathoracic volume, the patient can ventilate their lungs more effectively. However, they are not required in the respiration of a healthy individual, and so the use of accessory muscles is an important clinical sign of respiratory distress.
The scalene muscles are three paired muscles (anterior, middle and posterior), located in the lateral aspect of the neck. Collectively, they form part of the floor of the posterior triangle of the neck.
The scalenes act as accessory muscles of respiration, and perform flexion at the neck.
In this article, we shall look at the anatomy of the scalene muscles – their attachments, function, innervation and clinical importance. 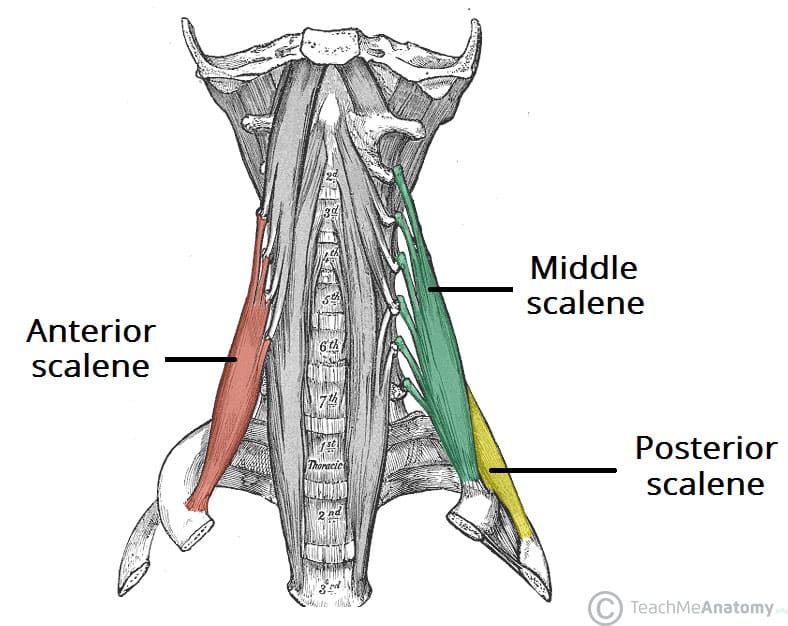
The anterior scalene muscle lies on the lateral aspect of the neck, deep to the prominent sternocleidomastoid muscle.
The middle scalene is the largest and longest of the three scalene muscles. It has several long, thin muscles bellies arising from the cervical spine, which converge into one large belly that inserts into the first rib.
The posterior scalene is the smallest and deepest of the scalene muscles. Unlike the anterior and middle scalene muscles, it inserts into the second rib.
The scalene muscles are an important part of the anatomy of the neck, with several important structures located between and around them.
The brachial plexus and subclavian artery pass between the anterior and middle scalene muscles. This provides an important anatomical landmark in anaesthetics for performing an interscalene block.
The subclavian vein and phrenic nerve pass anteriorly to the anterior scalene – the subclavian vein courses horizontally across it, while the phrenic nerve runs vertically down the muscle. The subclavian artery is located posterior to the anterior scalene. [caption id="attachment_10110" align="aligncenter" width="732"] Fig 2 – Proximal portion of the brachial plexus, in the neck. [start-clinical]
FAQ
What muscle passes through the scalene gap?
It descends along the side of the vertebral column to insert by a broad attachment into the upper surface of the first rib, posterior to the subclavian groove. The brachial plexus and the subclavian artery pass anterior to it.
What nerve pierces the middle scalene muscle?